Dispatches: Former Pro Diagnosed With COVID-19
As of this writing, roughly 2.1M people have been infected with the coronavirus worldwide, according to the World Health Organization, and as the pandemic continues to spread, COVID-19 is something that will likely change the rhythm of our world and our sport for a very long time.
We’ve connected with a handful of triathletes—each in very different geographical areas, with different athletic experience levels, and in different coronavirus situations. They range from international-level pros to age-groupers to coaches to college athletes. We initially collected six firsthand experiences as the pandemic fully hit the U.S. a few weeks ago, but as the virus continues to expand, we’ll be also featuring a wider scope of affected triathletes.
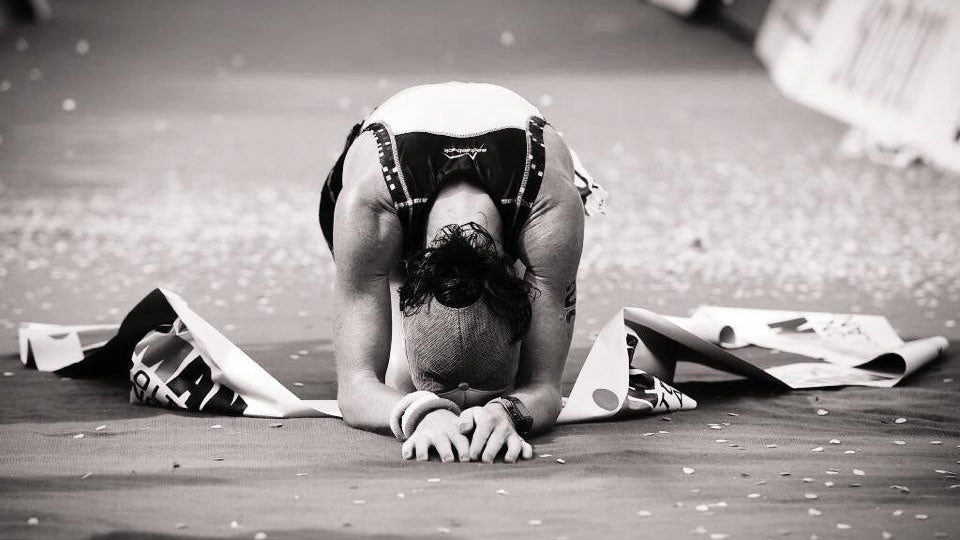
Today, we’re checking in with Dr. Tamsin Lewis, a 40-year-old medical doctor, former pro triathlete, and 2014 Ironman UK champion. Though Dr. Lewis resides in London, she is currently in Devon recovering from a severe case of COVID-19 that she contracted in March from an unknown source. Though the worst of her symptoms have passed, she is still coping with the disease’s impact and her inability to fully recover.
As of this writing, the United Kingdom has approximately 103,000 cases of COVID-19 and just under 14,000 deaths, according to the World Health Organization, putting the country at a case rate of roughly 163 per 100,000 (for reference, the United States’ case rate is at roughly 208 per 100,000 people), yet the U.K. has a death rate nearly double that of the U.S. (22 per 100,000 people versus the 10 per 100,000, respectively).
On Her Current Area’s Restrictions:
“I live in London, but I came to Devon (countryside in southwest of U.K) shortly before we went into lockdown, near my parents home and where I grew up.
“I was not aware I had coronavirus at the time, but could see that we may follow the course of Italy, so I wanted to be out of the city. London has been hit very badly. We are all on lockdown—essential travel only, supermarkets and pharmacies are open, but distancing is enforced. No exercise facilities are open, we’re allowed out for exercise once a day, and only with one member of the household—not in groups, and it’s been patrolled very vigilantly by the police.”
On Contracting Coronavirus:
“I’m a medical doctor, I was living in central London, I was traveling on public transport, seeing multiple clients who travel internationally. I had returned from Thailand in mid-January. I had an unusual chest infection at the end of January, so it weakened my defenses…
“The virus hit me hard, I developed a secondary pneumonia and struggled to breathe for a week. I was monitored at home by doctors remotely but did go to hospital for a scan and blood tests. I am now four weeks in; it’s been a bumpy course, two steps forward, one step back.”
On Her Symptoms:
“The first night, I could feel my heart racing, then I developed some stomach cramps, and chills. My Oura ring (a device that tracks sleep, heart-rate variability, body temperature, and more) gave me a red flag that my body temperature was up 3 degrees F, and my heart rate was elevated.
“That was the first time I thought, ‘Hm, this might be something.’ I’ve had that before, this was nothing new, but the fatigue I felt was extraordinary. The tightness in my chest evolved over the next seven days, and the cough was very light, but I had this really heavy aching and soreness in my joints—specifically in my hip flexors and my lower back, despite not doing any exercise. It was very tiring just to walk around, and we know that this deep muscle ache is a sign that one has contracted a more severe form of COVID-19.”
On The Recovery Process:
“I first had a test for the coronavirus about ten days after I got symptoms, and that came back as positive. By that time, I had started to get a bit better, and I went for a long walk and tried to do a bit of a run, but ended up that evening with a fever again, lots of joint swelling in my hips and knees again. So it set me hugely back, and that’s something that I want to really highlight: If you get this virus or assume you get this virus, as soon as you exercise you will likely set yourself back. You have to take it super super easy. I learned the hard way. My heart was racing—a resting heart rate of 40 became 75. It was astonishing.
“Especially if you have severe symptoms like chest symptoms and these deep muscle aches. It is frustrating but patience really is important. This is not a virus to mess with. You do not want long term complications. Athletes need their lungs!”
On Her Treatment:
“I was treated symptomatically for pain, with a mix of paracetamol and codeine. Avoid NSAIDS like Voltaren and Ibuprofen. I had an antibiotic for the chest symptoms, I also had three days of the malarial drug Hydroxyquinone, but I did not tolerate it well at all—it gave me tinnitus, dropped my blood glucose, and I think it caused some of the hyperactivity in my immune system that I’m experiencing now. [Quinone is] an immunosuppressant, so when you stop it, you can get a rebound inflammatory immune response. I also took high doses of vitamin C, but not as high doses as we now know is necessary to combat an infection (>10g/day). I was taking zinc, in the form of lozenges, Omega-3, turmeric, curcumin, NAC, Vitamin D. All of the above to help the immune system and counteract the inflammation side effects. They may have helped.
“I think it’s important for people to stop their iron supplements during this time—which I know a lot of athletes are on—because it can exacerbate the oxidative stress in the body, which this virus causes. I was also taking a sleep remedy by Doc Parsley with melatonin—it’s very hard to sleep with this illness, because of the compounded effects of anxiety about what is coming next and also the shortness of breath. I also took an antihistamine – chlorpheniramine – to help allergy symptoms and to help with calming.”
On The Effects Of The Virus:
“The worst point of this illness is really the severe pain I experienced in my hip flexors and my lower back, which is like nothing I’ve ever experienced, even after running an Ironman. It was a very deep, stabbing pain. Secondarily, the sensation of not being able to breathe. I think as athletes sometimes we take our lungs for granted, and I certainly never thought I’d be unwillingly out of breath walking up the stairs, while having to use the banister, for weeks…It feels like you’ve done three Ironmans in a row every day, plus not being able to breathe, and that’s not really very nice. Not everyone suffers it like this, but I do think my history of extreme endurance athleticism, accompanied by a tendency to under-fuel/recover in the past has affected my immune system, so I want to encourage restorative practices in these times to improve your immunity. It’s also a good time to get a blood screen to check for anemia, vitamin D and B12 levels as these can hamper your ability to deal with the virus.”
On Being An Athlete With Coronavirus:
“I think what I’ve learned is that if you ask for any medical help, the medics don’t as a rule compute that you have so much reserve as an athlete in your lungs and in your heart. My resting heart rate was elevated from 40 to 80, and yet it wasn’t taken seriously because that was in the normal range—but that certainly wasn’t the normal range for me. We know our baselines are different, so please get to know YOUR normal and communicate that to caregivers. Given that I had healthy lungs, my oxygen saturation that I was measuring through this p02 fingertip device didn’t really go down that much, even though I was experiencing shortness of breath and a tight chest—we’re very efficient as athletes at extracting oxygen from the blood. That’s only the case if you’re not anaemic, so if you suspect this, please get a simple commercially available CBC blood test.”
On What Surprised Her, As A Doctor:
“We’re all kind of learning and in this together as medics because we really don’t know how to treat this yet. We know how to support. I’m in a number of groups with a number of healthcare professionals who are all trying to figure out what works, what doesn’t, and we are trialling different medicines in different cohorts of people rapidly. I encourage people not to self medicate with drugs like the malarial drug because there are side effects.”
On What Triathletes Need To Know:
“They really need to take it easy if they get infected. It’s worth having a blood test to check on immunity and other factors I’ve mentioned before, and they really need to prioritize the restorative recuperative aspect of exercise if you’re training during this time: Prioritizing refueling in the window after exercise when your immunity is most compromised is important in that 90-minute post exercise window; avoiding long duration (over 60 minutes) fasted training is not recommended either.
“There can be lasting damaging effects from this illness—like my experience with inflammation and joint pain a month down the line. I’m being forced to see a rheumatologist to explore whether the virus has triggered off an autoimmunity in my body. An unpredictable course in many.”
On What Worries Her:
“…people breaking quarantine to train together to think that they’re above this virus, that their immune systems are strong. This virus can affect anyone. Yes, it’s more likely to affect older people with health conditions, but it certainly can affect younger people and it can take you down. So please be careful. Observe the social distancing, and really eat well, try to sleep well, and measure your heart-rate variability to see how restored your nervous system is and therefore how recovered you are from whatever exercise and training you’ve been doing.”
On What She’s Looking Forward To:
“I’ve been thinking and dreaming of climbing the Alpe d’Huez again, and I was dreaming of all of the hills I’ve climbed on my bike. I’m certainly not interested in competing in the near future, and I’ve changed my outlook on what matters, so my competitive mindset has been forced to change. For me, it’s more about the journey than the destination and the enjoyment of the challenge rather than the placing. Returning to Ironman as an amateur after racing pro, I found I was just going through the motions, no real enjoyment—so new horizons, perhaps an XTERRA one day. This whole experience has forced me to look at how I live, what I value, and prioritise that concept I used to find nauseating: self-care.”